Summary
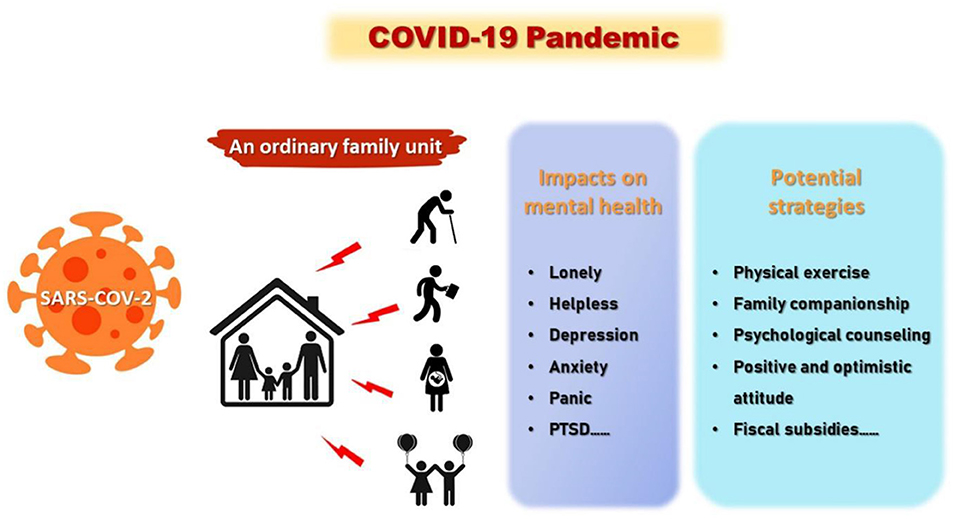
The COVID-19 pandemic has profoundly impacted mental health across the United States, sparking increases in anxiety, depression, and stress-related disorders. Social isolation, economic instability, and disruptions to daily life intensified psychological strain across demographics. This comprehensive guide explores these effects, evaluates coping strategies, and highlights emerging mental health solutions shaping America’s path to recovery.
Introduction: The Silent Mental Health Crisis
While COVID-19’s physical health consequences were widely reported, its psychological impact has been equally significant, though less visible. Social distancing, lockdowns, and fear of infection disrupted lives in ways that triggered stress, anxiety, and depression for millions of Americans. The Centers for Disease Control and Prevention (CDC) reported that over 40% of U.S. adults experienced symptoms of anxiety or depression in 2021—an alarming rise from pre-pandemic levels. This mental health crisis has affected nearly every age group and socio-economic demographic, demanding urgent attention and actionable solutions.
How COVID-19 Exacerbated Mental Health Challenges
Social Isolation and Loneliness
Lockdowns and social distancing measures were necessary to curb the spread of COVID-19, but they also severed crucial social connections. Individuals who were previously socially active found themselves confined to their homes, and many seniors faced extreme isolation in nursing homes. Research indicates that prolonged isolation doubles the risk of depression in older adults, while young adults suffered from anxiety stemming from lack of peer interaction.
Real-Life Example:
In New York, nursing home residents reported depression rates twice as high during lockdown periods, highlighting the severe psychological toll of social isolation.
Economic Stress and Unemployment
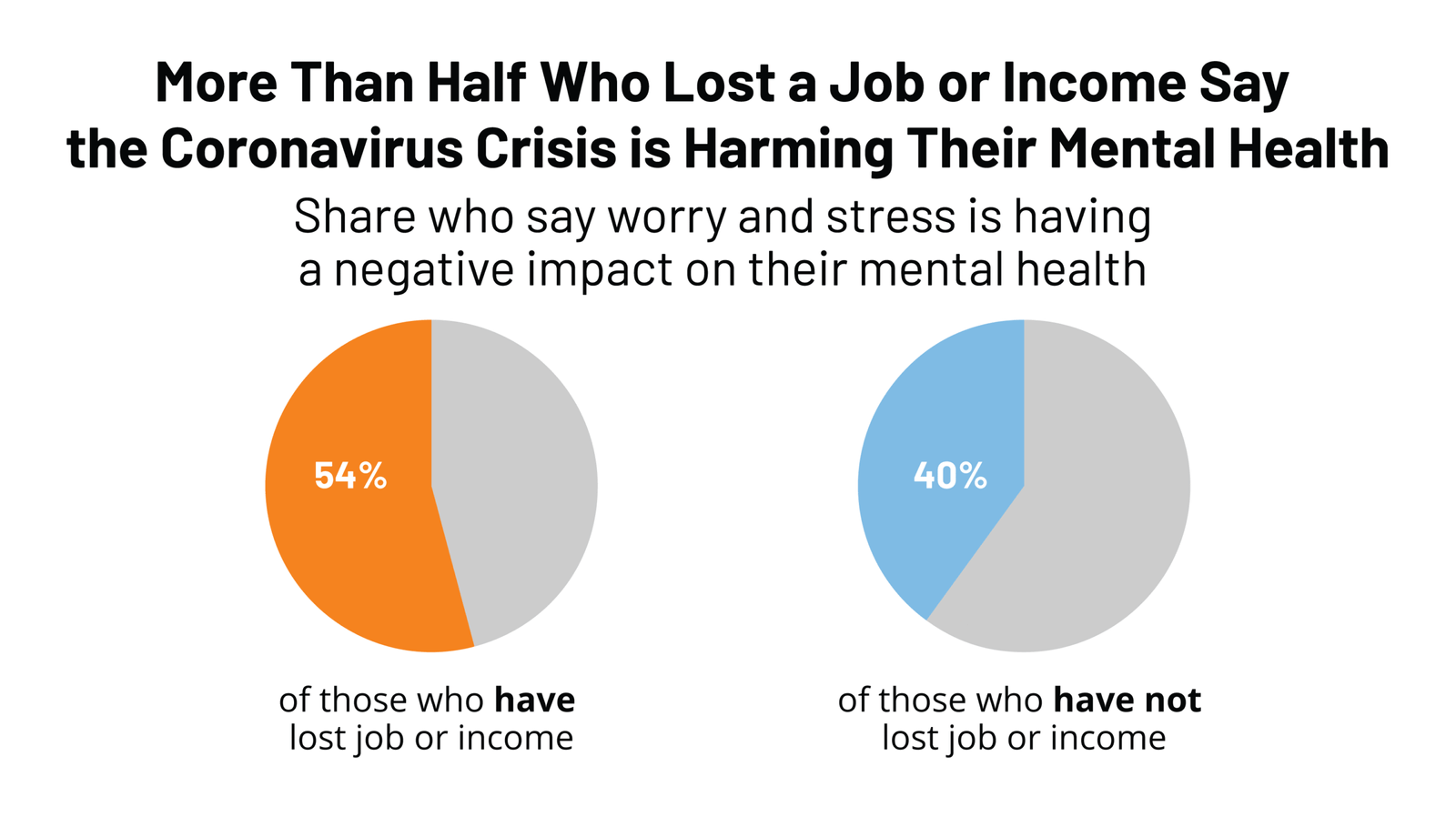
The economic ramifications of COVID-19 contributed significantly to mental health strain. Job losses, furloughs, and pay reductions led to financial anxiety and uncertainty. Freelancers and gig workers, who lacked the safety nets provided to full-time employees, were particularly vulnerable.
Real-Life Example:
Survey data from the CARES Act recipients revealed that financial stress was cited as the primary factor worsening mental health, with many reporting anxiety and disrupted sleep due to uncertain income.
Fear of Illness and Health Anxiety
Constant media coverage and the unpredictable nature of the virus generated widespread fear. Individuals with pre-existing health conditions or caregiving responsibilities experienced heightened health-related anxiety. The fear of contracting COVID-19 extended beyond personal health concerns to worries about loved ones, amplifying stress levels across households.
Disruption of Routine Mental Health Care
Lockdowns led to the temporary closure of mental health clinics, reducing access to therapy and counseling. While teletherapy services emerged as a solution, technological limitations and privacy concerns prevented some populations from fully utilizing these tools.
Population-Specific Impacts
Youth and Adolescents
Remote schooling introduced challenges such as excessive screen time, disrupted socialization, and academic pressure, contributing to stress and emotional fatigue. The CDC reported a 25% increase in emergency room visits for mental health among teens during the peak months of the pandemic. Adolescents struggled to adapt to the lack of routine and peer interaction, resulting in increased anxiety and depressive symptoms.
Frontline Workers
Healthcare providers were at the frontline, facing moral injury, trauma, and burnout. Long shifts, high patient mortality, and exposure to COVID-19 created extreme mental strain. Studies show ICU nurses and doctors reported PTSD-like symptoms, highlighting the urgent need for targeted psychological support.
Seniors
Older adults were particularly vulnerable due to isolation and heightened risk of infection. Extended periods of loneliness contributed to cognitive decline and depression. Telehealth services and virtual support partially alleviated these challenges, but many seniors still faced profound psychological effects.
Minority Communities
Structural inequalities meant that Black, Latino, and Native American communities experienced disproportionately high infection rates and limited access to care. This increased stress, anxiety, and the prevalence of mental health disorders in these groups, underscoring the need for culturally competent interventions.
Teletherapy and Digital Mental Health Solutions
The pandemic accelerated the adoption of teletherapy platforms like Talkspace, BetterHelp, and Headspace. These services provided a convenient, stigma-free way to access mental health support.
Benefits:
- Accessibility for remote or high-risk patients.
- Reduced stigma by allowing therapy from home.
- Continuity of care during lockdowns.
Challenges:
- Not all populations had access due to digital literacy or privacy issues.
- Complex or severe mental health cases may require in-person intervention.
Pointers:
- Approximately 50% of U.S. adults utilized teletherapy services at least once during the pandemic.
- Teletherapy allowed patients to maintain treatment plans, preventing regression for many mental health conditions.
Coping Mechanisms and Wellness Practices
Americans adopted various wellness strategies to mitigate pandemic-induced stress.
- Mindfulness and Meditation: Apps like Calm and Headspace surged in popularity.
- Exercise and Outdoor Activities: Physical activity helped alleviate anxiety and depressive symptoms.
- Community Support: Virtual support groups reduced feelings of isolation and provided emotional relief.
- Routine Building: Maintaining daily schedules helped individuals manage stress and increase resilience.
Key Takeaways:
- Consistent daily routines contribute to mental stability.
- Professional intervention remains essential for severe mental health issues.
- Public education campaigns can help reduce stigma and encourage early help-seeking.
Long-Term Implications for U.S. Mental Health
The pandemic exposed systemic weaknesses in the mental health infrastructure.
- Rising Demand for Professionals: Mental health services require expansion to meet growing needs.
- Integration with Primary Care: Embedding mental health screening and services in primary care can improve accessibility.
- Insurance Reforms: Expanding coverage for mental health services will ensure more Americans can seek help.
- Public Awareness Campaigns: Education on coping strategies and mental health literacy is critical to post-pandemic recovery.
FAQs
- How has COVID-19 affected anxiety levels in Americans?
The pandemic led to a marked increase in anxiety disorders due to social isolation, financial instability, and health fears. Chronic stress, restlessness, and difficulty focusing became widespread, leading many to seek therapy or digital mental health tools as a means of coping with unprecedented uncertainty. - What populations were most affected by pandemic-related depression?
Young adults, frontline healthcare workers, seniors, and minority communities experienced the highest levels of depression. Disrupted routines, isolation, and systemic inequities contributed to significant mental strain, resulting in increased clinical diagnoses and highlighting the need for tailored intervention strategies. - Did teletherapy effectively replace in-person mental health services?
Teletherapy provided vital continuity of care during lockdowns. While it worked for many, access gaps, privacy concerns, and technology literacy issues limited its reach. Severe or complex cases often still required face-to-face therapy for comprehensive treatment and accurate diagnosis. - How did remote learning impact children and adolescents?
Remote learning caused increased stress and anxiety among youth. Limited social interaction, academic pressure, and screen fatigue contributed to emotional exhaustion. Virtual counseling services provided some relief, but the lack of in-person socialization left lasting effects on mental well-being. - What role did financial stress play in mental health during COVID-19?
Financial instability, job losses, and economic uncertainty fueled anxiety and depressive symptoms. Economic stress led to sleep disruptions, increased substance use, and heightened overall psychological distress, emphasizing the interplay between economic security and mental wellness. - Are healthcare workers experiencing long-term mental health effects?
Yes. Frontline workers reported burnout, PTSD-like symptoms, and moral injury. Continuous exposure to high-risk environments and patient deaths created lasting psychological strain, necessitating comprehensive support systems and counseling programs for healthcare professionals. - How did seniors cope with isolation during the pandemic?
Many seniors used digital communication tools to maintain connections, though access and digital literacy were barriers. Community outreach programs and telehealth services partially mitigated loneliness, but social isolation still contributed to depression, cognitive decline, and reduced overall well-being among elderly populations. - Did minority communities face unique mental health challenges?
Yes. Systemic inequities, healthcare disparities, and higher infection rates heightened stress in Black, Latino, and Native American populations. Targeted outreach, culturally competent counseling, and community support are critical to addressing these disparities and ensuring equitable mental health care access. - Which wellness practices were most effective during COVID-19?
Mindfulness, meditation, structured routines, exercise, and outdoor activities significantly alleviated stress and anxiety. Participation in virtual social support networks helped reduce isolation, demonstrating the importance of holistic wellness practices in maintaining mental health during crises. - What long-term strategies can improve U.S. mental health post-pandemic?
Expanding mental health infrastructure, integrating services into primary care, promoting teletherapy, and providing equitable access are essential. Public education campaigns to reduce stigma, alongside professional support services, will enhance mental health resilience and ensure better preparedness for future crises.
Conclusion:
The COVID-19 pandemic has illuminated the fragility and importance of mental health in American society. Rising rates of anxiety, depression, and stress highlight the need for systemic change, increased access to care, and innovative solutions. By embracing technology, promoting wellness practices, and expanding equitable mental health services, the U.S. can mitigate long-term psychological consequences and build a resilient population prepared for future challenges.