For decades, the term “self-care” was often relegated to the realms of scented candles, indulgent baths, and guilty pleasures—a nice-to-have, but non-essential luxury. Meanwhile, the American healthcare system operated on a predominantly reactive model: you get sick, you see a doctor, you receive treatment. This “sick-care” system, while brilliant at acute intervention and trauma care, has proven increasingly strained, expensive, and ill-equipped to handle the slow, rising tide of chronic disease.
Today, a profound shift is underway. Self-care is being redefined not as an indulgence, but as a fundamental pillar of health, grounded in rigorous scientific evidence and holistic principles. It is evolving from a buzzword into a disciplined practice, one that is actively reshaping our understanding of health, wellness, and the very structure of healthcare delivery in America. This is not a rejection of conventional medicine, but a powerful integration with it—a move towards a proactive, personalized, and participatory model of health where the individual is an active agent in their own well-being.
The Paradigm Shift: From Sick-Care to Health-Care
The statistics are sobering. According to the Centers for Disease Control and Prevention (CDC), chronic diseases such as heart disease, cancer, diabetes, and obesity are the leading causes of death and disability in the United States, accounting for 90% of the nation’s $4.1 trillion in annual healthcare expenditures. These conditions are largely driven by modifiable lifestyle factors: diet, physical activity, tobacco use, and alcohol consumption.
The reactive “sick-care” model, focused on pharmaceutical and surgical interventions after a disease has manifested, is like mopping the floor while the sink overflows. It addresses symptoms but often misses the underlying causes. This has created an unsustainable cycle of rising costs, physician burnout, and patient dissatisfaction.
Enter the science of self-care. This new paradigm is built on a foundation of prevention and proactive maintenance. It recognizes that the daily choices we make—what we eat, how we move, how we sleep, and how we manage stress—directly influence our biological functioning at a cellular level, altering our risk for chronic disease and our overall quality of life. This is not alternative medicine; it is the very essence of preventive medicine, now armed with a growing body of evidence from fields like epigenetics, psychoneuroimmunology, and nutritional biochemistry.
The Evidence-Based Pillars of Holistic Self-Care
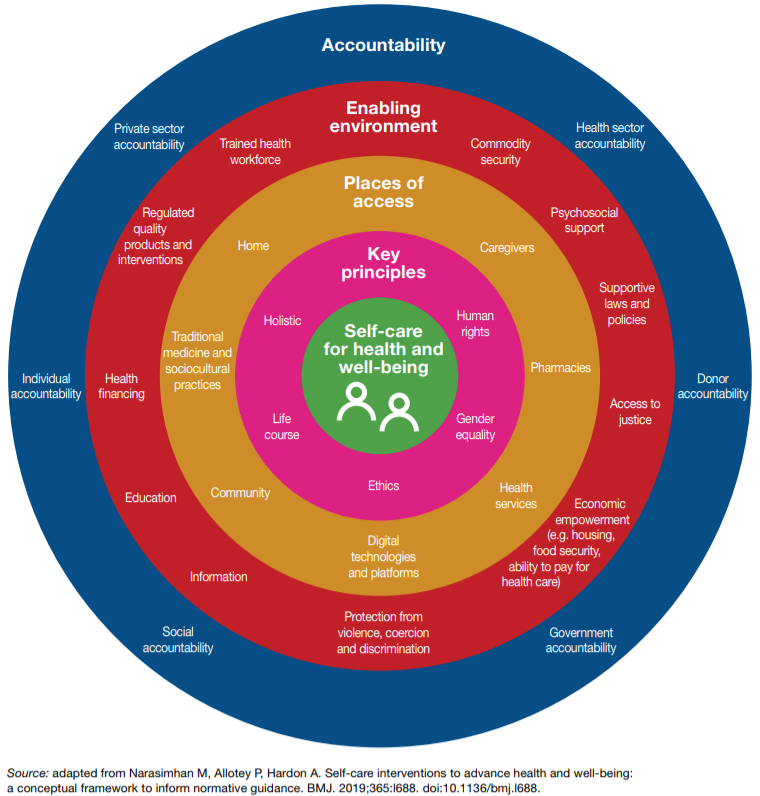
Holistic self-care acknowledges that the mind and body are not separate entities but an intricately connected system. What affects one, inevitably affects the other. The following pillars are not just “good ideas”; they are non-negotiable biological requirements for health, each supported by a robust body of scientific literature.
Pillar 1: Nutritional Psychiatry and the Gut-Brain Axis
The old adage, “you are what you eat,” has been upgraded by science to “your brain is what you eat.” The field of nutritional psychiatry has exploded, revealing the profound connection between our diet, our gut microbiome, and our mental health.
- The Mechanism: The gut is often called the “second brain” because it produces a vast array of neurotransmitters, including about 95% of the body’s serotonin, a key regulator of mood, sleep, and appetite. This communication happens via the gut-brain axis, a bidirectional superhighway linking the emotional and cognitive centers of the brain with peripheral intestinal functions.
- The Evidence: Large-scale studies, such as the SMILES trial, have demonstrated that a Mediterranean-style diet—rich in fruits, vegetables, whole grains, lean protein, and healthy fats—can be as effective as psychotherapy or medication in treating moderate to severe depression. Conversely, diets high in processed foods, sugar, and unhealthy fats are consistently linked to an increased risk of depression, anxiety, and even cognitive decline.
- The Self-Care Application: Evidence-based self-care means viewing food as medicine. It involves prioritizing a diverse, plant-rich diet to cultivate a healthy gut microbiome, incorporating fermented foods for probiotics, and consuming adequate fiber to feed beneficial gut bacteria (prebiotics). This is not about restrictive fad diets, but about nourishing the ecosystem within us to directly support neurological and psychological health.
Pillar 2: The Physiology of Mindfulness and Stress Reduction
Stress is not just a feeling; it is a measurable physiological state. When we perceive a threat, our body releases cortisol and adrenaline, initiating the “fight-or-flight” response. While essential for survival in acute situations, chronic stress keeps this system activated, leading to systemic inflammation, elevated blood pressure, impaired immune function, and damage to the hippocampus, a brain region critical for memory and learning.
- The Mechanism: Mindfulness practices, such as meditation, deep breathing, and yoga, act as a counterbalance, activating the parasympathetic nervous system—the “rest-and-digest” response. Research using fMRI technology shows that regular meditation can physically change the brain, increasing gray matter density in areas associated with emotional regulation and self-awareness while decreasing it in the amygdala, the brain’s fear center.
- The Evidence: A meta-analysis published in JAMA Internal Medicine concluded that mindfulness meditation programs can improve anxiety, depression, and pain. Studies from Harvard and the University of Wisconsin have shown that these practices can reduce the expression of pro-inflammatory genes and improve immune response to vaccines. The American Heart Association has issued a statement endorsing meditation as a complementary approach to lower cardiovascular risk.
- The Self-Care Application: Evidence-based stress reduction moves beyond “just relax.” It involves the deliberate, daily practice of techniques that recalibrate the nervous system. This could be a 10-minute daily meditation using a validated app like Insight Timer or Calm, a mindful walking practice, or a structured program like Mindfulness-Based Stress Reduction (MBSR). The goal is to build resilience by changing our relationship with stress, not necessarily eliminating it.
Pillar 3: Exercise as a Multisystem Therapy
The benefits of exercise extend far beyond weight management. Physical activity is one of the most potent, scientifically-proven tools we have for enhancing overall health and preventing disease.
- The Mechanism: Exercise induces the release of myokines, molecules released by muscle cells that have hormone-like effects. These molecules reduce inflammation, improve insulin sensitivity, and promote brain health. Exercise also boosts levels of brain-derived neurotrophic factor (BDNF), a protein that supports the survival of existing neurons and encourages the growth of new ones, acting like fertilizer for the brain.
- The Evidence: The science is unequivocal. The American College of Sports Medicine positions exercise as a primary therapy for conditions ranging from type 2 diabetes and osteoarthritis to depression and anxiety. Studies show that regular physical activity can be as effective as antidepressant medication for mild to moderate depression. It improves sleep quality, enhances cognitive function, and is linked to a reduced risk of numerous cancers.
- The Self-Care Application: The “no pain, no gain” mentality is being replaced by a more nuanced understanding. The key is consistency and finding a form of movement you enjoy. The CDC recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week, plus muscle-strengthening activities. This could be brisk walking, cycling, dancing, or strength training. The focus is on making movement a non-negotiable part of the daily routine, akin to brushing one’s teeth.
Pillar 4: The Non-Negotiable Nature of Sleep
Sleep is perhaps the most underappreciated pillar of health. It is not a passive state but an active and critical period of restoration, memory consolidation, and metabolic cleanup for the brain and body.
- The Mechanism: During deep sleep, the brain’s glymphatic system becomes highly active, clearing out metabolic waste products like beta-amyloid, which is associated with Alzheimer’s disease. Sleep is also crucial for hormonal regulation; it balances ghrelin and leptin (hunger hormones), supports immune function, and consolidates learning and memory.
- The Evidence: Chronic sleep deprivation (consistently less than 7 hours per night for adults) is strongly linked to an increased risk of obesity, heart disease, stroke, dementia, and depression. The World Health Organization has classified night shift work as a probable carcinogen due to the disruption of circadian rhythms. Research from the University of California, Berkeley, has shown that a single night of poor sleep can increase anxiety levels by up to 30%.
- The Self-Care Application: Scientific self-care treats sleep with the seriousness it deserves. This involves practicing good “sleep hygiene”: maintaining a consistent sleep schedule, ensuring the bedroom is cool and dark, avoiding blue light from screens for at least an hour before bed, and limiting caffeine and alcohol intake. Tracking sleep with wearable technology can also provide valuable data and motivation.
Read more: Mind, Body, Spirit: Integrating Ancient Wisdom with Modern American Life
The Integration: How Self-Care is Reshaping the Healthcare System
This groundswell of evidence is not happening in a vacuum. It is actively being integrated into the fabric of American healthcare, changing how providers practice and how patients engage with their health.
- The Rise of Lifestyle Medicine: This is an official medical specialty that uses therapeutic lifestyle interventions as a primary modality to treat chronic conditions. Board-certified Lifestyle Medicine physicians are trained to help patients make and sustain behavior changes in the six pillars: a whole-food, plant-predominant eating pattern, physical activity, restorative sleep, stress management, positive social connections, and avoidance of risky substances. This is conventional medicine fully embracing the science of self-care.
- The Proliferation of Digital Health Tools: Wearables (like Fitbit, Oura Ring, and Whoop) and health apps provide individuals with unprecedented data about their own bodies—from heart rate variability (a marker of stress resilience) and sleep cycles to activity levels. This data empowers people to make informed, personalized decisions and provides objective feedback that motivates sustained behavior change. Telehealth platforms also make it easier to access coaches, dietitians, and mental health professionals who specialize in these holistic methods.
- A New Model of the Patient-Provider Relationship: The traditional, paternalistic model of “doctor knows best” is evolving into a collaborative partnership. In this new model, the patient is an active participant. They come to appointments with data from their wearables, questions about lifestyle interventions, and a willingness to co-create a treatment plan. The physician’s role expands from diagnostician and prescriber to coach, educator, and partner.
- Economic Incentives and Value-Based Care: As the healthcare system slowly shifts from fee-for-service (paying for procedures) to value-based care (paying for outcomes), there is a powerful financial incentive to keep people healthy. Hospitals and insurance companies are increasingly investing in wellness programs, health coaching, and nutritional counseling because it is more cost-effective to prevent a heart attack than to treat one.
A Word of Caution: Navigating Misinformation and Ensuring Safety
The popularity of holistic health has, unfortunately, created a fertile ground for misinformation. It is crucial to approach self-care with a critical and evidence-based mindset.
- Distinguish Between Science and Anecdote: A celebrity endorsement or a single personal success story is not scientific evidence. Look for large, randomized controlled trials, systematic reviews, and meta-analyses published in peer-reviewed journals.
- Beware of “Miracle Cures”: If it sounds too good to be true, it probably is. Health is complex and multifaceted; there are no simple, one-size-fits-all solutions.
- Consult Your Healthcare Provider: The most important principle of evidence-based self-care is that it complements, never replaces, conventional medical care. Always discuss new supplements, major dietary changes, or new exercise regimens with your doctor, especially if you have a pre-existing condition or are taking medication.
Conclusion: The Future is Proactive, Personalized, and Participatory
The science of self-care represents a quiet revolution. It is a return to the foundational principles of health, now supercharged by 21st-century science and technology. It empowers us with the knowledge that we have more agency over our health and well-being than we may have previously believed.
This shift is moving us away from a fragmented, disease-centered system and toward a holistic, patient-centered one. The future of American healthcare is not just in the development of new drugs or sophisticated surgical techniques, but in the widespread adoption of daily, evidence-based self-care practices that prevent disease before it starts. It is a future where each of us is the primary steward of our own health, supported by a healthcare system that finally lives up to its name: a system designed to help us care for our health, not just treat our sickness.
Read more: Beyond the Pill: A Beginner’s Guide to Holistic Healing Practices in the USA
Frequently Asked Questions (FAQ)
Q1: This all sounds time-consuming. How can I possibly fit all of this into my already busy schedule?
This is one of the most common and valid concerns. The key is to start small and view self-care as a cumulative practice, not an all-or-nothing endeavor. You do not need to meditate for an hour, run 5 miles, and cook a gourmet organic meal every day.
- Micro-habits are powerful: A 5-minute meditation, a 10-minute walk, swapping a sugary snack for a piece of fruit—these small, consistent actions add up significantly over time.
- Stack your habits: Link a new habit to an existing one. For example, do 5 minutes of deep breathing after you brush your teeth in the morning. Or, take a work call while walking outside.
- Prioritize: View these practices not as optional extras, but as essential maintenance for your most valuable asset: your health. It’s about quality and consistency, not quantity.
Q2: Isn’t “holistic” just a code word for “unscientific” or “alternative”?
Not anymore. While the term has been co-opted by some non-evidence-based practices, its core meaning—addressing the whole person (mind, body, spirit) rather than just symptoms—is now at the forefront of scientific medical fields like Psychoneuroimmunology (studying the mind-immune system connection) and Lifestyle Medicine. The mechanisms by which mindfulness changes the brain, diet affects mood, and sleep cleanses toxins are now measurable and being rigorously studied at major academic institutions worldwide.
Q3: How do I know if a wellness trend or supplement is evidence-based or just a fad?
Develop your critical thinking skills. Ask these questions:
- What is the source? Is the information from a reputable institution like a university, a major hospital, or a government health agency (e.g., NIH, CDC)? Or is it from a blog trying to sell you something?
- Is it based on a single study or a body of research? One study is a starting point, not proof. Look for consensus from multiple, high-quality studies.
- Are the claims dramatic and oversimplified? Be wary of phrases like “miracle cure,” “reverse disease overnight,” or “one weird trick.” Real science is complex and rarely offers magic bullets.
- Talk to a professional: Your doctor or a registered dietitian can help you navigate the evidence and determine what is safe and appropriate for you.
Q4: I have a chronic medical condition. Is it safe for me to engage in these practices?
Absolutely, and it may be even more beneficial. However, the “consult your doctor” rule is paramount. For instance:
- Someone with diabetes needs to work with their doctor or dietitian to ensure dietary changes align with their blood sugar management.
- Someone with a physical injury needs clearance from a physical therapist before starting a new exercise regimen.
- Those with serious mental health conditions should use mindfulness as a complement to, not a replacement for, therapy and/or medication.
A good healthcare provider will welcome your interest in lifestyle interventions and help you integrate them safely into your overall treatment plan.
Q5: What is the single most impactful change I can make to start?
While the pillars are interconnected, if we had to pick one with the most widespread and immediate benefits, it would be improving sleep quality. Sleep is the foundation upon which all other self-care is built. When you are well-rested, you have better emotional regulation to manage stress, more energy to exercise, and clearer judgment to make healthy food choices. Prioritizing 7-9 hours of quality sleep per night can create a positive ripple effect across every other area of your health. Start there.