Taking the step to seek support for your mental and emotional well-being is one of the most powerful decisions you can make. Yet, in the complex landscape of American healthcare, figuring out where to turn can feel overwhelming. You’re faced with a confusing array of titles: Therapist, Psychologist, Psychiatrist, LCSW, LMHC, Coach… What do they all mean? How are they different? And most importantly, which one is right for you?
The choice isn’t just about credentials; it’s about finding the right type of support for your unique needs, goals, and circumstances. Seeing the wrong professional can lead to frustration, wasted time and money, and can even discourage you from continuing your search.
This guide is designed to demystify the process. We will break down the roles, responsibilities, training, and costs of each type of mental health professional in the USA. Our goal is to empower you with the knowledge and confidence to take the next step on your wellness journey, ensuring you connect with the support that will be most effective for you.
Part 1: The Core Differences – A High-Level Overview
Before diving into the details, let’s start with a simple analogy and a clear table.
The Restaurant Analogy:
- A Psychiatrist is like a master chef and nutritionist who focuses on the biological ingredients of your meal. They diagnose complex dietary needs, prescribe specific medicinal ingredients (like supplements or specialized foods), and monitor your body’s physiological response. They ensure the fundamental biochemical foundation is correct.
- A Therapist is like a skilled cooking coach who teaches you how to cook. They help you understand recipes (coping skills), work through your fear of the stove (past trauma), improve your technique (behavioral change), and create a sustainable, enjoyable cooking practice for life. They focus on the “how-to” of daily living.
- A Coach is like a motivational meal-planner who helps you achieve a specific culinary goal, like running a 5k or eating more vegetables. They provide accountability, structure, and strategies to overcome plateaus. They are future-oriented and action-focused, but they don’t diagnose or treat underlying eating disorders.
Now, let’s look at the data:
| Professional | Core Focus | Can Diagnose? | Can Prescribe Medication? | Typical Approach | Best For… |
|---|---|---|---|---|---|
| Psychiatrist | Biological, medical | Yes | Yes | Medication management, medical interventions | Severe mental illness (Bipolar, Schizophrenia), complex cases, medication needs |
| Psychologist | Psychological, testing | Yes | No (in most states) | In-depth therapy, psychological assessment | Diagnosis clarification, deep trauma work, personality disorders |
| Therapist/Counselor | Emotional, behavioral | Yes | No | Talk therapy, skill-building, coping strategies | Anxiety, depression, life transitions, relationship issues, daily coping |
| Coach | Goal-oriented, future-focused | No | No | Action plans, accountability, achieving specific goals | Achieving career, fitness, or life goals (non-clinical) |
The Golden Rule: If you are experiencing significant distress, dysfunction, or symptoms that interfere with your daily life (sleep, work, relationships), starting with a licensed therapist or psychiatrist is the safest and most recommended path.
Part 2: Deep Dive into the Roles
1. The Therapist (The Heart of Talk Therapy)
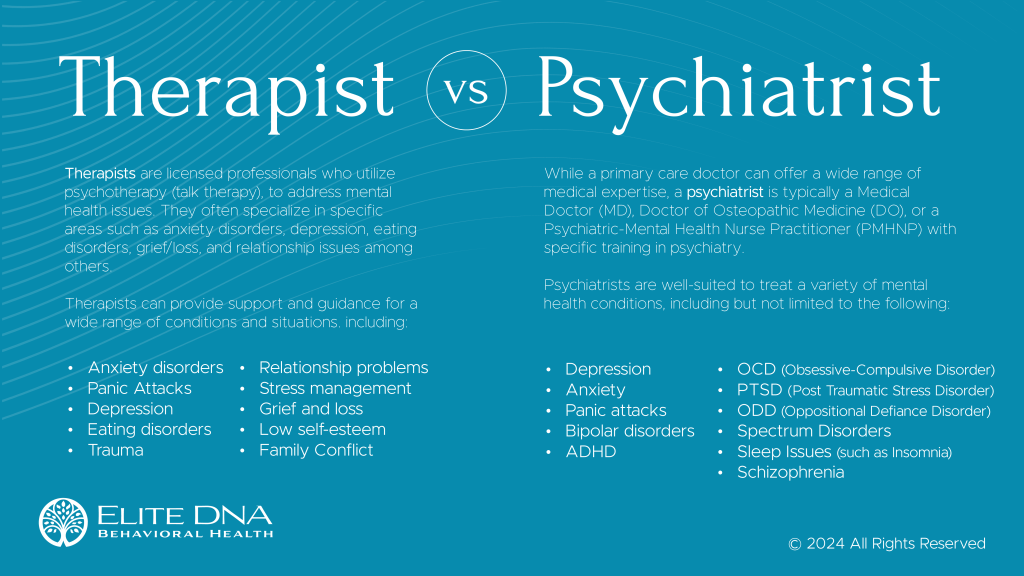
“Therapist” is an umbrella term for a licensed professional trained to provide psychotherapy (talk therapy). They hold at least a Master’s degree and are regulated by a state licensing board.
Common Titles and Credentials:
- Licensed Clinical Social Worker (LCSW): Trained in therapy with a deep understanding of how environmental and systemic factors (family, community, society) impact mental health. They are often skilled in navigating community resources.
- Licensed Professional Counselor (LPC) or Licensed Mental Health Counselor (LMHC): Hold a master’s degree in counseling and are trained in a variety of therapeutic techniques to address mental health and wellness.
- Marriage and Family Therapist (LMFT): Specializes in treating individuals, couples, and families from a relational and systems perspective. They view problems as patterns within a relationship system rather than just within an individual.
What They Do:
Therapists provide a confidential, non-judgmental space to explore your feelings, thoughts, and behaviors. They help you:
- Understand and process past trauma or difficult life events.
- Develop coping skills for anxiety, depression, and stress.
- Navigate life transitions (grief, divorce, career change).
- Improve communication and relationship skills.
- Identify and change negative thinking and behavioral patterns.
- Manage and reduce symptoms of diagnosed mental health conditions.
When to See a Therapist:
- You’re feeling stuck, overwhelmed by sadness, worry, or anger.
- You’re going through a painful life transition or have experienced trauma.
- Your relationships are consistently strained or unfulfilling.
- You’re struggling with a specific mental health condition like an anxiety disorder, depression, or PTSD.
- You want to understand yourself better and build emotional resilience.
2. The Psychiatrist (The Medical Expert)
A psychiatrist is a medical doctor (MD or DO) who specializes in the diagnosis, treatment, and prevention of mental, emotional, and behavioral disorders. Their training is primarily medical and biological.
What They Do:
- Medical Diagnosis: They conduct comprehensive psychiatric evaluations to diagnose complex mental health conditions like Major Depressive Disorder, Bipolar Disorder, Schizophrenia, and ADHD.
- Medication Management: This is their primary role. They prescribe psychotropic medications (antidepressants, mood stabilizers, antipsychotics, etc.) and manage the dosage and combinations based on your symptoms and side effects.
- Medical Monitoring: They order and interpret medical tests (e.g., blood tests) to rule out physical causes for psychiatric symptoms (e.g., thyroid issues causing depression) and to monitor the physical impact of medications.
- Psychotherapy: Some psychiatrists are also trained in therapy and may provide it, but due to high demand and insurance structures, most focus on medication management and may work in tandem with a therapist.
When to See a Psychiatrist:
- You suspect you have a complex condition that may require medication (e.g., severe depression, Bipolar Disorder).
- Your therapist or primary care physician recommends a medication evaluation.
- You are already on medication and need your prescription managed or adjusted.
- You are experiencing severe symptoms that significantly impair your ability to function (e.g., psychosis, mania, severe suicidal thoughts).
3. The Psychologist (The Assessment and Therapy Specialist)
A psychologist holds a Doctorate degree (PhD or PsyD) in psychology. Their training is heavily focused on research, psychological theory, and advanced therapeutic techniques.
What They Do:
- Psychological Testing and Assessment: This is a key differentiator. Psychologists administer and interpret sophisticated tests to diagnose learning disabilities, cognitive decline, brain injuries, ADHD, and personality disorders. This provides a detailed, data-driven picture of your functioning.
- Psychotherapy: They provide in-depth, evidence-based therapy, often for complex cases. Many specialize in specific modalities like psychoanalysis or dialectical behavior therapy (DBT) for borderline personality disorder.
- Research and Academia: Many psychologists work in research settings, universities, or hospitals, contributing to the scientific understanding of mental health.
When to See a Psychologist:
- You or your child need comprehensive psychological testing for a clear diagnosis (e.g., for an IEP at school, or to clarify a complex diagnosis).
- You are seeking a specific, intensive form of therapy for a complex condition like trauma or a personality disorder.
- You have not found success with other therapeutic approaches and want a deeper, more assessment-driven approach.
4. The Coach (The Action-Oriented Partner)
A coach is an unregulated professional who focuses on personal and professional development. There are no universal educational or licensing requirements, though many pursue certifications from various coaching federations.
What They Do:
Coaches are future-focused and goal-oriented. They partner with you to:
- Clarify and achieve specific personal or professional goals (e.g., career change, starting a business, improving fitness).
- Identify and overcome self-imposed obstacles and limiting beliefs.
- Create actionable plans and provide structure and accountability.
- Maximize potential and performance in various areas of life.
Critical Distinction: Coaching vs. Therapy
- Therapy often looks backward to understand and heal the why behind current struggles (e.g., “Why does criticism trigger me?” linked to a past wound).
- Coaching looks forward to strategize and achieve the what (e.g., “What steps can I take to become more resilient to criticism in my career?”).
When to See a Coach:
- You are generally mentally healthy but feel stuck or unmotivated in achieving a specific goal.
- You want to improve your performance in a particular area of your life (leadership, productivity, health).
- You desire accountability and a structured process to create change.
- Important: Coaching is not appropriate for treating mental illness, trauma, or deep-seated psychological pain.
Read more: The Benefits of Meditation for Mental Health
Part 3: A Step-by-Step Guide to Making Your Choice
Use this flowchart to guide your decision-making process.
Step 1: Assess Your Symptoms and Goals
Ask yourself:
- Are my symptoms severe? (e.g., inability to get out of bed, thoughts of harming myself or others, hearing voices, extreme mood swings). -> Start with a Psychiatrist.
- Am I struggling with diagnosed or suspected clinical issues? (e.g., persistent anxiety, depression, PTSD, OCD, eating disorders). -> Start with a Therapist.
- Do I need clarity on a diagnosis? (e.g., “Do I have ADHD or is it anxiety?”). -> Consider a Psychologist for testing or a Psychiatrist for a medical diagnosis.
- Am I functionally well but want to achieve more? (e.g., career advancement, better work-life balance, building confidence for public speaking). -> Consider a Coach.
Step 2: Understand the Practicalities
- Insurance and Cost:
- Psychiatrists, Psychologists, and Therapists are often covered by health insurance, though copays and deductibles apply. You must check if they are “in-network.” Without insurance, psychiatrists are often the most expensive.
- Coaches are almost never covered by health insurance and are paid out-of-pocket.
- The Collaboration Model: It is extremely common, and often ideal, for people to see both a therapist (for weekly talk therapy and skills) and a psychiatrist (for monthly medication management). They work as a team to support your care.
Step 3: Find a Provider – Where to Look
- Your Insurance Company’s Directory: The most practical first step. This lists in-network providers.
- Online Therapist Directories:
- Psychology Today: The largest and most popular directory. You can filter by location, insurance, specialty, and issue.
- Therapy for Black Girls / Therapy for Latinx: Culturally sensitive directories for communities of color.
- Open Path Collective: A nonprofit offering low-cost therapy sessions ($40-$70) for individuals in financial need.
- Referrals:
- Ask your Primary Care Physician (PCP) for a referral.
- Ask trusted friends or family.
- University Training Clinics: Local universities with psychology or counseling programs often have low-cost clinics staffed by supervised graduate students.
Step 4: The Consultation – Your “First Date”
Most providers offer a brief (15-20 minute) phone consultation. This is your chance to interview them. Prepare questions:
- “Do you have experience treating [my specific issue, e.g., social anxiety]?”
- “What is your therapeutic approach? (e.g., CBT, psychodynamic, etc.)”
- “What are your fees, and do you accept my insurance?”
- “What is your availability? Do you have openings for new clients?”
- “How do you typically work with clients? What can I expect from our sessions?”
Step 5: Evaluate the Fit – The “It Factor”
The most important factor in successful therapy is the therapeutic alliance—the relationship between you and your provider. After your first session, ask yourself:
- Did I feel heard, respected, and understood?
- Did I feel safe and comfortable being open?
- Does their communication style work for me?
- Do I feel hopeful about working with this person?
It is perfectly okay to try one or two sessions and decide it’s not a good fit. You have the right to find someone else. A good professional will not take this personally and may even help you with a referral.
Part 4: A Glossary of Common Therapeutic Approaches
You may hear these terms during your search. Here’s a simple breakdown:
- Cognitive Behavioral Therapy (CBT): A practical, present-focused therapy that helps you identify and change negative thought patterns and behaviors that contribute to your distress. Highly effective for anxiety and depression.
- Dialectical Behavior Therapy (DBT): A type of CBT that emphasizes balancing acceptance and change. It teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Often used for Borderline Personality Disorder but now applied more broadly.
- Psychodynamic Therapy: Explores how unconscious processes and past experiences (often from childhood) shape your current behavior and relationships. It’s more about self-understanding than quick skills.
- Eye Movement Desensitization and Reprocessing (EMDR): A specialized therapy used primarily to treat PTSD. It involves using bilateral stimulation (like eye movements) to help the brain process and heal from traumatic memories.
- Humanistic / Person-Centered Therapy: Focuses on your inherent capacity for growth and self-actualization. The therapist provides empathy and unconditional positive regard, creating a supportive environment for you to find your own solutions.
Conclusion: Your Journey, Your Choice
The path to mental wellness is not a one-size-fits-all highway; it’s a personal journey with different guides for different parts of the trek. You might start with a therapist to build coping skills, consult a psychiatrist for medication to stabilize a biological condition, and later work with a coach to achieve new heights once you’re on solid ground.
The most important step is the first one: deciding that you deserve support. By understanding the distinct roles of psychiatrists, therapists, psychologists, and coaches, you can move forward not with confusion, but with clarity and confidence. You are the expert on your own life. Now, you have the knowledge to find the right professional expert to partner with you.
Remember, finding the right fit is a process, not a single event. Be patient and persistent. The investment you make in your mental health is the most valuable investment you will ever make, and the right support system can make all the difference.
Frequently Asked Questions (FAQ)
Q1: Can my Primary Care Physician (PCP) prescribe mental health medication?
A: Yes, many PCPs do prescribe common antidepressants and anti-anxiety medications, especially for mild to moderate cases. This can be a great and accessible first step. However, for complex conditions, medication-resistant symptoms, or the need for controlled substances (like stimulants for ADHD), they will typically refer you to a psychiatrist, who has more specialized training.
Q2: What’s the difference between a “therapist” and a “counselor”? Is one better?
A: The terms are often used interchangeably. Both are licensed professionals who provide psychotherapy. The difference is usually in their academic training (e.g., a Counselor may have a Master’s in Counseling, while a Social Worker has a Master’s in Social Work). The specific license (LCSW, LPC, LMFT) and the individual clinician’s experience and approach are more important than the title itself.
Q3: How long does therapy typically take to work?
A: There is no standard timeline. Some people experience relief after just a few sessions of learning new skills, while others may engage in therapy for years to work through deep-seated trauma or patterns. It depends on your goals, the nature of your issues, and your level of engagement. A good therapist will discuss treatment goals and expectations with you early on.
Q4: I’m concerned about the cost. What are my options for affordable care?
A: There are several avenues to explore:
- Insurance: Use in-network providers to significantly reduce costs.
- Sliding Scale: Many private practice therapists offer reduced fees based on your income. Always ask.
- Community Mental Health Centers: These are federally funded to provide care regardless of ability to pay.
- University Clinics: As mentioned, these offer low-cost services from supervised trainees.
- Online Therapy Platforms: Some platforms can be more affordable than traditional private practice, but research their privacy policies and quality of care.
Q5: Is online therapy (teletherapy) as effective as in-person therapy?
A: A large body of research now shows that for most common issues like anxiety and depression, teletherapy is just as effective as in-person therapy. It also offers greater convenience and access for people in rural areas or with mobility issues. The most important factor remains the quality of the relationship with your provider, regardless of the medium.
Q6: What should I do if I don’t feel a connection with my therapist?
A: This is a common and valid experience. The therapeutic relationship is unique, and not every pairing will be a good fit. It is perfectly appropriate and encouraged to address this directly. You can say, “I appreciate our work together, but I’m not sure the fit is right for me. I would like to discuss ending our sessions and/or getting a referral.” A professional and ethical therapist will respect this decision and help you transition. Do not feel obligated to stay out of politeness; your healing is the priority.